Liver Cirhhosis
A Comprehensive Guide to Causes, Symptoms, and Treatment
The liver is the powerhouse of your body, performing hundreds of essential tasks from filtering toxins to aiding digestion. But when it suffers long-term damage, it can lead to a serious condition called cirrhosis. Liver cirrhosis is the late-stage scarring (fibrosis) of the liver, where healthy tissue is gradually replaced by non-functional scar tissue, impairing its ability to work properly.
Understanding this condition is the first step toward managing it effectively. As a dedicated medical centre in Ahmedabad, we are committed to providing patients with the knowledge and advanced care needed to manage liver disease. This guide covers the critical aspects of liver cirrhosis, from its causes and symptoms to the latest treatment approaches available today.
What is Liver Cirrhosis?
Common Causes of Liver Cirrhosis in India
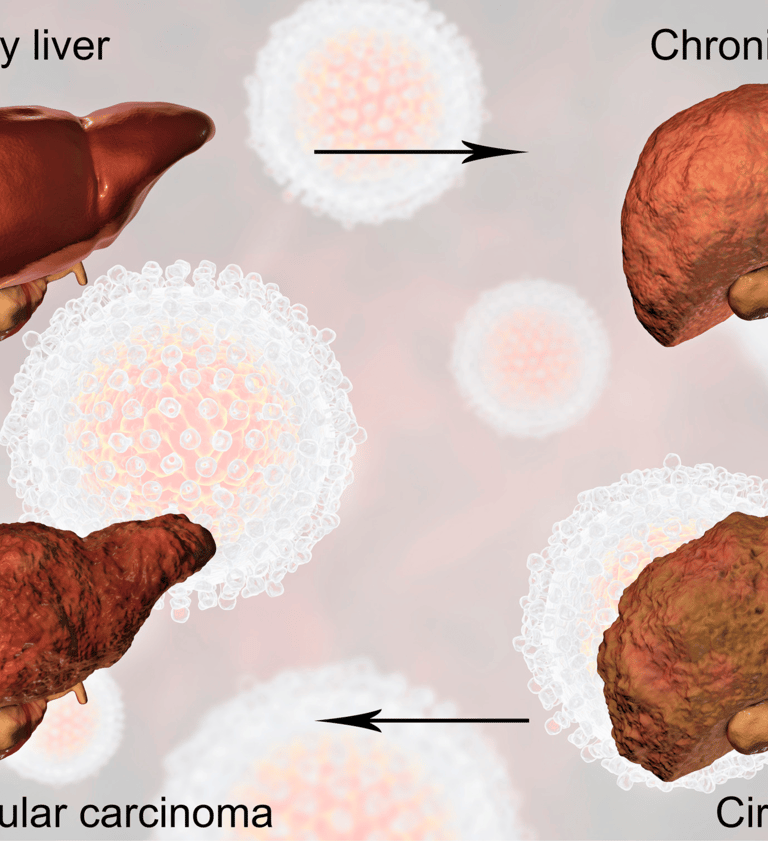
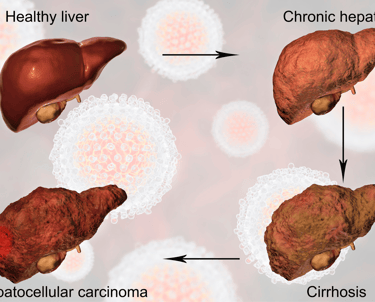
Think of cirrhosis as the result of a continuous battle within your liver. Whenever your liver is injured, it tries to repair itself. In this process, scar tissue forms. When the injury is chronic and repetitive—due to factors like long-term alcohol abuse or viral infections—the scar tissue builds up extensively. This advanced scarring is known as cirrhosis. It stiffens the liver, disrupts its internal structure, and severely hampers blood flow, leading to a progressive loss of liver function
Early Stage (Compensated) Cirrhosis Symptoms
Diagnosis and Staging
Advanced Stage (Decompensated) Cirrhosis Symptoms
Alcoholic Liver Disease: Chronic, excessive alcohol consumption is a leading cause of cirrhosis.
Chronic Viral Hepatitis (B and C): Long-term infection with the Hepatitis B or C virus causes sustained inflammation that leads to scarring.
Non-Alcoholic Fatty Liver Disease (NAFLD): Now a rapidly growing cause, NAFLD is linked to obesity, diabetes, high cholesterol, and metabolic syndrome. It progresses from fat accumulation (fatty liver) to inflammation (NASH) and finally to cirrhosis.
Autoimmune Hepatitis: A condition where the body's own immune system mistakenly attacks and inflames the liver.
Genetic and Inherited Diseases: Conditions like Hemochromatosis (excess iron buildup) and Wilson's disease (excess copper buildup) can damage the liver.
Bile Duct Disorders: Diseases that block or damage the bile ducts, such as primary biliary cholangitis (PBC), can cause bile to back up and lead to cirrhosis.
When they do appear, they are often vague:
Feeling tired and weak
Loss of appetite and unexplained weight loss
Nausea and stomach discomfort
Red, blotchy palms
As liver function deteriorates, more severe and noticeable symptoms develop:
Jaundice: Yellowing of the skin and whites of the eyes.
Ascites: Fluid buildup causing swelling in the abdomen.
Edema: Fluid retention leading to swelling in the legs, ankles, and feet.
Easy Bruising and Bleeding: The liver produces fewer proteins needed for blood clotting.
Hepatic Encephalopathy: Confusion, drowsiness, memory loss, and slurred speech due to the buildup of toxins in the brain.
Intense Itching (Pruritus): Caused by bile products depositing in the skin.
Dark Urine and pale-coloured stools.
Blood Tests: Liver Function Tests (LFTs), kidney function tests, viral markers for hepatitis, and clotting profiles provide a clear picture of how the liver is performing.
Imaging Tests: An Ultrasound, CT Scan, or MRI can show the size, shape, and texture of the liver and detect complications like ascites or liver cancer.
FibroScan (Transient Elastography): A modern, non-invasive ultrasound-based test that measures the stiffness of the liver, providing an accurate assessment of scarring without a biopsy.
Liver Biopsy: A small sample of liver tissue is removed and examined under a microscope. This is the gold standard for confirming cirrhosis and determining its cause and extent.
Liver Cirrhosis Treatment: Managing the Condition
While the scarring from cirrhosis is generally irreversible, treatment can slow or halt its progression, manage symptoms, and prevent life-threatening complications.
Treating the Underlying Cause: This is the most important step.
Complete abstinence from alcohol.
Antiviral medications to eliminate Hepatitis B or C.
Weight loss, diet, and exercise to manage NAFLD.
Medications to suppress the immune system in autoimmune hepatitis.
Managing Complications:
Dietary Changes: A low-sodium diet is crucial to control fluid retention (ascites and edema).
Medications: Diuretics ("water pills") to remove excess fluid, and medications like lactulose to help reduce toxin buildup from hepatic encephalopathy.
Screening: Regular screening for liver cancer (hepatocellular carcinoma) and esophageal varices (swollen veins in the esophagus) is vital.
Liver Transplant: For end-stage liver failure where the liver has stopped functioning, a liver transplant is the only definitive cure.
My Office
Shalby Hospitals, Naroda, Ahmedabad.
Department of Gastrointestinal and HBP Sciences
Superspecialist GI-HBP Surgeon
Dr. Maunil Tomar
Gastro Oncosurgeon
Advanced Endoscopist
Contact
+91 9979591922
maunilgastro@gmail.com
